Robotic Joint Replacement Surgery
Mako robotic-assisted arthroplasty has transformed the landscape of joint replacement surgery by offering a level of precision and personalization that was previously unattainable with conventional techniques. Using a combination of 3D CT-based preoperative planning and intraoperative real-time guidance, Mako technology ensures improved outcomes and higher patient satisfaction. Here’s a comprehensive overview of the advantages of Mako robotic-assisted joint replacement:
Accuracy
Unmatched Surgical Precision & Accuracy
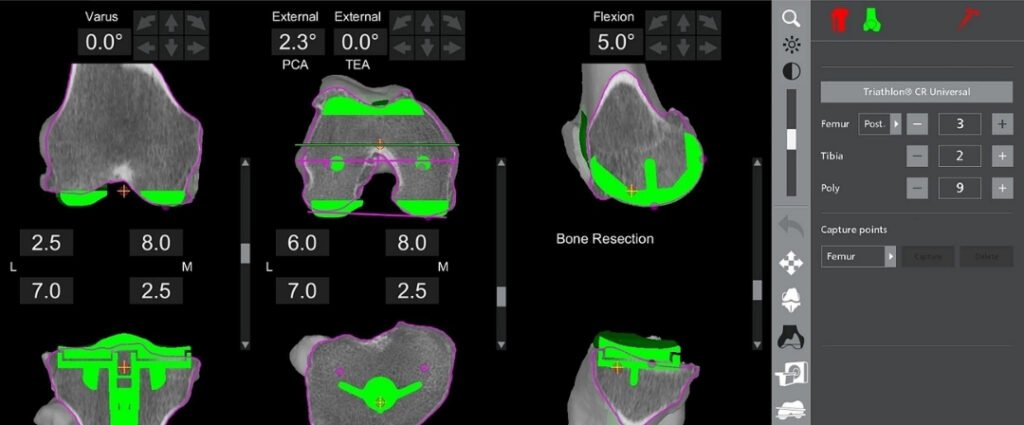
Mako technology allows the surgeon to create a personalized preoperative plan based on a CT scan of the patient’s joint. This 3D model helps map the exact anatomy, accounting for variations in bone structure and deformity.

During surgery, the robotic arm assists the surgeon with bone preparation and implant positioning, ensuring optimal alignment and reducing the risk of malalignment.

Studies have shown that Mako-assisted knee and hip replacements achieve up to 4 times greater accuracy in implant positioning compared to conventional techniques.
Improved Implant Longevity & Stability

Proper alignment and accurate implant placement significantly reduce uneven wear on the implant, extending its lifespan.

A study published in The Journal of Arthroplasty demonstrated that Mako-assisted knee arthroplasty led to a reduction in early aseptic loosening and enhanced implant durability due to better load distribution.
Reduced Risk of Soft Tissue & Ligament Injury

Mako technology enables real-time intraoperative adjustments to protect surrounding soft tissue and ligaments. This reduces the risk of inadvertent damage and postoperative instability.

Soft tissue balance is maintained with high precision, leading to improved functional outcomes and reduced risk of ligament-related complications.
Faster Recovery & Reduced Postoperative Pain

With improved accuracy in bone cuts and less trauma to surrounding tissues, patients experience reduced post-surgical pain and inflammation.

Multiple studies have reported that patients undergoing Mako-assisted arthroplasty have shorter hospital stays and require fewer opioid medications postoperatively.

A randomized controlled trial showed a 15-20% reduction in postoperative pain scores with Mako-assisted total knee replacement.
Lower Risk of Complications
Personalized Joint Replacement for Better Functionality
Proven Clinical Outcomes & High Patient Satisfaction

A multicenter study comparing Mako-assisted total knee replacement with conventional techniques found superior functional scores (KOOS and WOMAC) in the Mako group at 6 and 12 months postoperatively.

Hip replacement patients have also reported faster return to normal activities and better range of motion following Mako-assisted procedures.
Ideal for Complex Cases & Pre-Existing Hardware

Mako robotic-assisted arthroplasty is particularly beneficial in complex cases, including patients with pre-existing femoral or tibial hardware.

The system’s precise planning and controlled bone cuts allow for the safe retention of hardware while achieving.

Optimal implant positioning, reducing the need for hardware removal and associated complications.
Minimized Blood Loss & Reduced Need for Transfusion


JOINT REPLACEMENT SURGEON
DR. RUSHAY BHALODIYA
- A Mako Robotic-Assisted Joint Replacement Surgeon focused on knee, partial knee, and hip arthroplasty.
- More than 2000 robotic surgeries done with great accuracy and achieved excellent outcomes for the patients.
- Skilled in difficult and revision joint replacements, guaranteeing proficient use of the prosthetic with maximum survivorship.
- Innovating surgery performed in an outpatient setting dural decreases the time to recover as well as the precision of the surgery.






